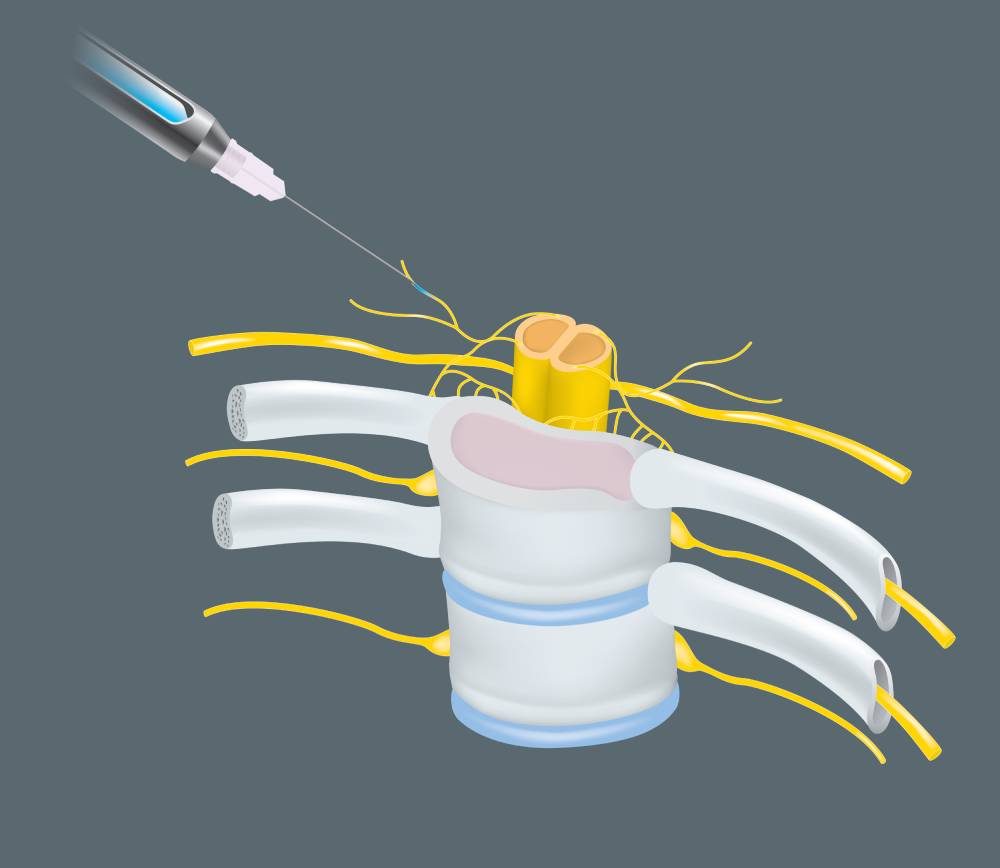
Rebound pain following nerve block represents a significant challenge in postoperative pain management. This phenomenon is characterized by a marked increase in pain intensity once the effects of regional anesthesia wear off. Rebound pain can significantly impact patient comfort and recovery, leading to increased opioid consumption and potential complications. Nerve blocks are a popular method for providing anesthesia and analgesia during and after various surgical procedures. They involve the injection of local anesthetics near specific nerves, temporarily inhibiting nerve function and thus blocking pain signals. The primary advantage of nerve blocks is their ability to offer targeted pain relief, reduce opioid requirements, and improve patient satisfaction in the immediate postoperative period (1). Despite these benefits, the subsequent onset of rebound pain poses a substantial challenge.
The mechanisms underlying rebound pain after nerve block are complex and not entirely understood. One theory suggests that the abrupt cessation of the anesthetic effect leads to a rapid return of nociceptive input, previously suppressed by the block, resulting in heightened pain perception. Furthermore, there is evidence indicating that the period of anesthesia may result in the upregulation of pain pathways, which can increase sensitivity when the block wears off (2). Additionally, local anesthetics may induce changes in both the peripheral and central nervous systems, contributing to an exacerbation of pain upon withdrawal (3).
Effective management of rebound pain requires a multifaceted approach, starting with preventive strategies. Multimodal analgesia, which combines different classes of analgesics, can provide synergistic pain relief that does not rely as heavily on one approach. Analgesic drugs can include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and gabapentinoids, which have been shown to reduce the severity of rebound pain (4). Continuous nerve block techniques, in which a catheter is placed for continuous local anesthetic infusion, can maintain consistent analgesia and reduce the incidence and severity of rebound pain (2).
Pharmacologic approaches to reduce rebound pain continue to evolve. Local anesthetics such as bupivacaine and ropivacaine are being evaluated for their duration of action and potential to cause rebound pain. Adjusting the concentration and volume of these anesthetics and exploring combinations with adjuvants such as dexmedetomidine or clonidine have shown promise in prolonging analgesia and reducing rebound pain intensity (3). However, individual patient variability requires a tailored approach that takes into account factors such as pain threshold, type of surgery, and overall health status.
Psychological factors also have a significant impact on the perception of rebound pain. Anxiety, depression, and previous pain experiences can increase rebound pain after nerve block. Cognitive-behavioral strategies, including preoperative counseling and postoperative support, have been suggested to help patients manage pain more effectively. These strategies aim to reduce the psychological impact of pain and improve overall pain management outcomes (1).
Future research is essential to further elucidate the mechanisms underlying rebound pain and to develop more effective prevention and treatment strategies. Studies focusing on the pharmacokinetics of different local anesthetics, the role of nerve block duration, and patient-specific risk factors for rebound pain could provide valuable insights. In addition, exploration of alternative regional anesthesia techniques and novel analgesic agents may improve postoperative pain management protocols.
In conclusion, rebound pain after nerve blockade is a significant challenge in postoperative pain management. Although the exact mechanisms remain unclear, this phenomenon is well documented and can lead to significant patient discomfort and increased opioid consumption. Effective management requires a comprehensive approach that includes multimodal analgesia, continuous nerve block techniques, and thorough patient education. Continued research and clinical innovation are critical to improving outcomes for patients who experience rebound pain after nerve block.
References
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131-157. doi:10.1016/j.jpain.2015.12.008
- Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011;113(4):904-925. doi:10.1213/ANE.0b013e3182285e01
- Lavand’homme P. Rebound pain after regional anesthesia in the ambulatory patient. Curr Opin Anaesthesiol. 2018;31(6):679-684. doi:10.1097/ACO.0000000000000651
- Lirk P, Picardi S, Hollmann MW. Local anaesthetics: 10 essentials. Eur J Anaesthesiol. 2014;31(11):575-585. doi:10.1097/EJA.0000000000000137